When reviewing medical reports, an intriguing term often surfaces: borderline EKG. But what does this term really signify? For those unacquainted with electrocardiograms (EKGs), the prospect of interpreting such findings can be daunting. However, understanding borderline EKG results could illuminate significant insights about one’s cardiovascular health and overall well-being.
First, it’s essential to grasp the foundational purpose of an EKG. An electrocardiogram captures the electrical activity of the heart over a period. The heart generates electrical impulses that trigger each heartbeat, flowing rhythmically and ensuring optimal blood circulation. An EKG serves as a vital diagnostic tool to gauge heart health, representing the heart’s rhythm and rate, the size and position of the heart chambers, and any potential disruptions in the heart’s electrical system.
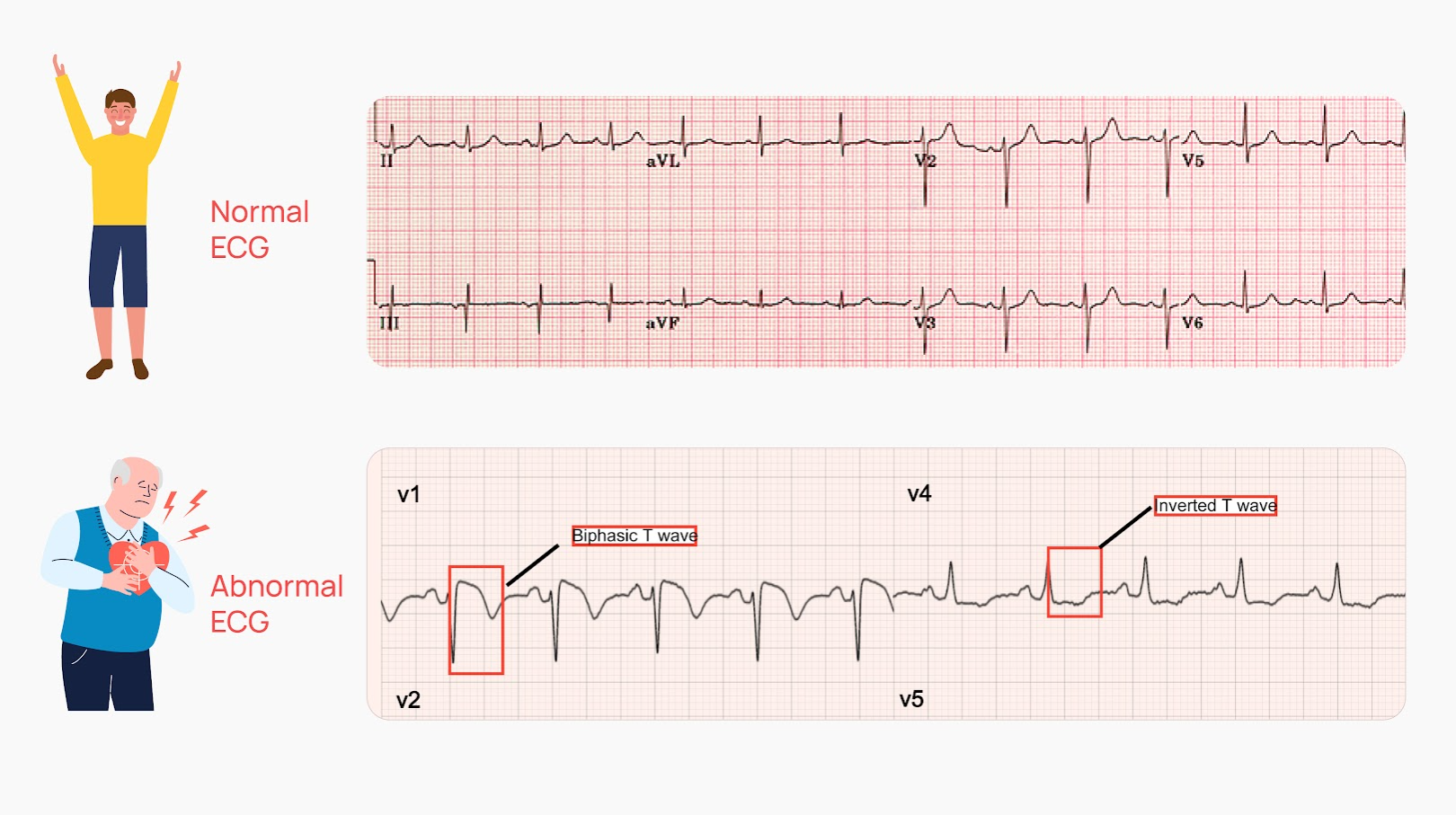
When interpreting EKG results, medical practitioners look for specific indicators that suggest normal functioning or potential abnormalities. A healthy EKG pattern usually displays a predictable set of waves that represent the heart’s electrical cycles—P waves, QRS complexes, and T waves—all grouped to signify the heart’s contractions and relaxations. However, when the findings reveal a “borderline” designation, it adds a layer of complexity. It suggests that aspects of the EKG are neither unequivocally normal nor explicitly abnormal, leaving room for further deliberation.
This phenomenon can stem from various scenarios. Borderline EKG readings may indicate minor irregularities that do not fit neatly into the normal or abnormal categories. These discrepancies can originate from several factors including the patient’s age, sex, physical condition, or even temporary states such as stress. Thus, while a borderline EKG can trigger alarm bells, it often requires further exploration rather than immediate conclusion.
One must consider the characteristics of the variations prompting a borderline classification. Such instances may involve minor heart rate fluctuations, slight deviations in the heart’s rhythm, or atypical wave shapes. These factors could denote disturbances like premature ventricular contractions or a slight degree of atrial enlargement. However, they may also reflect benign physiological responses, particularly in younger individuals or athletes whose hearts may exhibit unique patterns due to high levels of fitness.
The interpretation of borderline findings takes us into the intricate world of medical diagnostics. Clinicians typically engage in a comprehensive evaluation, dissecting the EKG within the larger context of the patient’s medical history and symptoms. They weigh the implications of the borderline readings against clinical manifestations, such as chest pain or shortness of breath. This holistic perspective ensures that medical professionals are not merely reacting to numbers or waveforms but assessing the overarching well-being of their patients.
It is also interesting to note that advancements in technology and interpretative methodologies have transformed our understanding of borderline EKGs. With modern algorithms and artificial intelligence being integrated into diagnostic processes, the evaluation may benefit from enhanced accuracy and specificity. Nonetheless, the human element remains irreplaceable. The experienced eye of a trained cardiologist can discern subtleties that automated systems might overlook.
Amidst rising interest in cardiovascular health, there’s a growing awareness of the lifestyle factors influencing EKG results. Obesity, hypertension, diabetes, and sedentary lifestyles can exacerbate heart conditions that might manifest as borderline readings. This realization underscores the critical importance of preventative measures. Adopting a healthier lifestyle, including balanced nutrition, regular exercise, and stress management, can mitigate risks associated with borderline EKG findings and promote overall heart health.
When confronted with a borderline EKG result, patients often adopt a spectrum of emotional responses, from anxiety to indifference. The key here is fostering an informed and proactive mindset. Education regarding the implications of such results can empower patients to engage in discussions with healthcare providers about potential follow-up tests or lifestyle changes. This collaborative approach fosters a sense of agency in managing one’s cardiovascular health, transforming borderline results from a source of trepidation into a springboard for informed health decisions.
Furthermore, understanding the prevalence of borderline EKG results can shift one’s perspective significantly. Research indicates that borderline findings are relatively common, particularly among otherwise healthy populations. This statistic has important implications, as it suggests that encountering such results does not always herald a serious medical crisis. Instead, it might reflect the normal variability in human physiology, allowing room for greater awareness and less alarm.
Ultimately, addressing what a borderline EKG means invites a broader conversation about cardiovascular health, systemic wellness, and the integration of lifestyle choices. While a borderline reading may imply the necessity for further investigation or monitoring, it fundamentally serves as a reminder to remain vigilant and proactive about heart health. Understanding and interpreting these findings could not only enrich one’s perception of their health but could also spur transformative lifestyle changes that positively affect well-being long-term.
In conclusion, when navigating the intricacies of borderline EKG results, it is vital to embrace an informed perspective. Bridging the gap between clinical interpretation and personal health engagement can foster a holistic approach to cardiovascular wellness. So, the next time you come across the term “borderline EKG” in a medical report, remember that beneath that seemingly simple phrase lies a wealth of information worth exploring further.