In the intricate web of healthcare, where each thread signifies a different facet of patient care, understanding the nuances of the CMS HCC (Centers for Medicare & Medicaid Services Hierarchical Condition Categories) is essential. This system is not merely a bureaucratic coding exercise; it is a pivotal mechanism that underpins healthcare reimbursement and quality of care. To fathom the depths of CMS HCC, one must delve into its multifaceted layers, much like peeling back the delicate skin of an onion—each layer unveiling a new insight.
At its core, the CMS HCC model serves as an instrument for risk adjustment. It categorizes patient diagnoses into a hierarchical structure aimed at predicting costs and resource utilization. Picture a grand orchestra, where each musician must play their part harmoniously, creating a symphony of care that resonates throughout the healthcare system. CMS HCC is the conductor, guiding this ensemble to ensure that resources are allocated efficiently, aligning funds with the patients who need them most. With accurate coding and robust data, healthcare providers can secure the necessary reimbursement to maintain the quality of services offered to their patients.
The foundation of CMS HCC lies in its systematic approach to coding. It utilizes a complex algorithm that groups diseases and conditions according to their clinical implications and costs. This hierarchical structure allows for a deeper understanding of patient populations, effectively categorizing individuals who possess similar health characteristics. Think of it as a tapestry, where each thread corresponds to a specific condition. This tapestry represents the collective health of a population and aids insurers in making informed decisions about funding and provision of services.
Herein lies the intrigue of the CMS HCC model: it rewards accuracy and detail. Healthcare providers must document diagnoses meticulously, capturing the full spectrum of patient conditions—from chronic illnesses to acute events. Each entry in a patient’s medical record is akin to a brushstroke on a canvas; together, they create a vivid picture of health that informs not only reimbursement but also the broader narrative of a patient’s journey through the healthcare system. The more comprehensive and precise the documentation, the finer the art of healthcare delivery becomes.
Moreover, the categorization provided by CMS HCC extends beyond mere reimbursement. It serves as a compass, guiding healthcare providers in tailoring their services to meet the distinct needs of various patient demographics. For instance, patients with multiple chronic conditions require a different approach compared to those navigating isolated health challenges. The HCC model encourages a proactive stance, fostering care coordination and promoting preventative measures that can forestall adverse health outcomes. By viewing patients through the lens of HCC categories, providers can develop targeted interventions that enhance overall well-being.
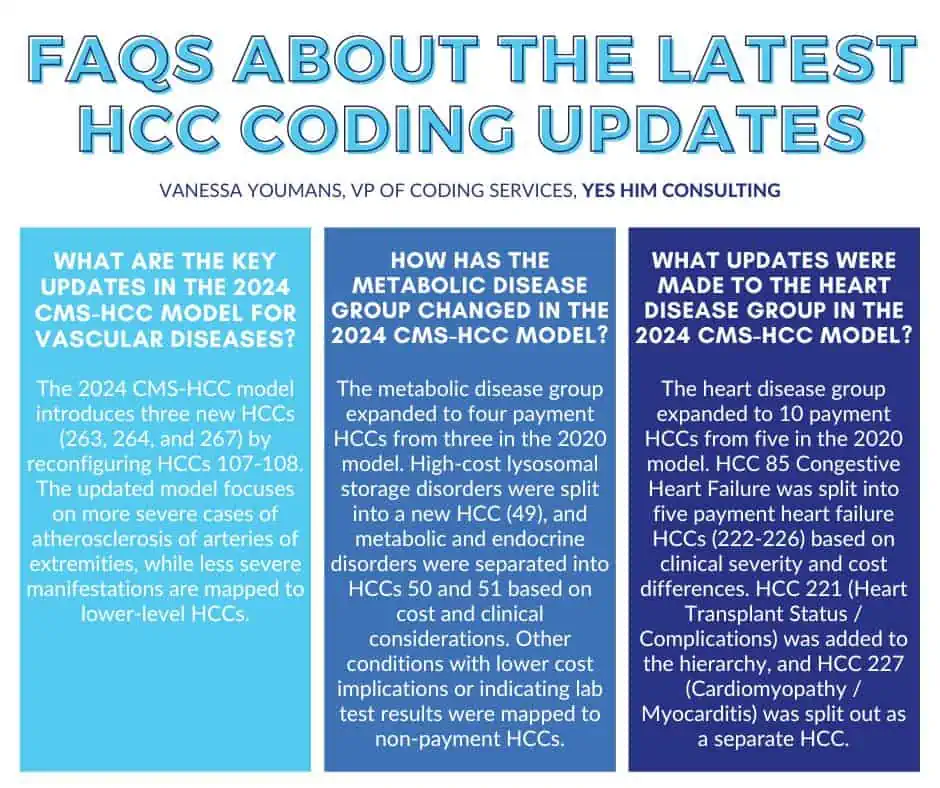
It is crucial to note that the HCC model is not static. Like the seasons, it evolves and adapts to the changing landscape of healthcare. The CMS regularly updates the categories, reflecting advancements in medical knowledge and shifts in demographic trends. This dynamic nature ensures that the coding system remains relevant, enabling healthcare systems to address emerging health challenges effectively. Therefore, staying abreast of these updates is vital for healthcare providers, who must navigate this ever-changing terrain while ensuring compliance and optimization of care delivery.
As we transition from the theoretical to the practical, the implementation of the CMS HCC model poses a distinct set of challenges. However, these challenges can be likened to climbing a formidable mountain—arduous, yet ultimately rewarding. Healthcare organizations must invest in training and resources to master the intricacies of accurate coding. This investment echoes the ethos of continuous improvement, whereby providers not only aim for compliance but also strive for excellence in the delivery of healthcare services. The rewards of such diligent efforts are manifold, including enhanced revenue streams, superior patient outcomes, and a well-coordinated care continuum.
Furthermore, engaging in regular audits and monitoring of coding practices can illuminate areas ripe for enhancement. These evaluations act as diagnostic tools—allowing organizations to identify discrepancies and rectify gaps in documentation. In the same way that a skilled artisan refines their craft through practice and reflection, healthcare providers can elevate their coding practices, fostering a culture of accountability and excellence.
In conclusion, understanding what CMS HCC means transcends mere theoretical knowledge; it embodies a comprehensive grasp of how healthcare systems function and flourish. This coding paradigm, rooted in the principles of risk adjustment, plays a quintessential role in steering the course of patient care and resource allocation. As healthcare navigators work to unravel the complexities of this model, they create pathways that lead to improved patient outcomes and a more sustainable healthcare system. Just as skilled artisans craft their masterpieces, healthcare providers, armed with the robust tools of CMS HCC, can forge a healthcare landscape that is responsive, equitable, and above all, compassionate.