In the intricate tapestry of healthcare, where every thread contributes to the overall picture of patient care, the terms CMS and HCC emerge as pivotal elements woven into the fabric of medical billing. Understanding these concepts is akin to deciphering a complex code, unlocking the secrets to financial reimbursement for healthcare providers while ensuring that patients receive the necessary care they need. This exploration will delve into what CMS and HCC mean in medical billing, examining their significance, structure, and implications for providers and patients alike.
Understanding CMS
At the core of the medical billing universe is the Centers for Medicare & Medicaid Services (CMS), a federal agency that plays a cardinal role. Much like a central bank regulates the flow of currency, CMS governs the intricate financial transactions of healthcare. This agency is responsible for overseeing the Medicare and Medicaid programs, which provide essential health services to millions of Americans, including the elderly, disabled, and low-income individuals.
Just as a conductor harmonizes the disparate elements of an orchestra, CMS establishes guidelines, regulations, and payment structures that unify the actions of healthcare providers across the nation. The agency’s policies affect nearly every facet of medical billing, guiding how services are coded, billed, and reimbursed. Understanding CMS not only illuminates the mechanics of the billing process but also reveals the underlying principles of healthcare finance and access.
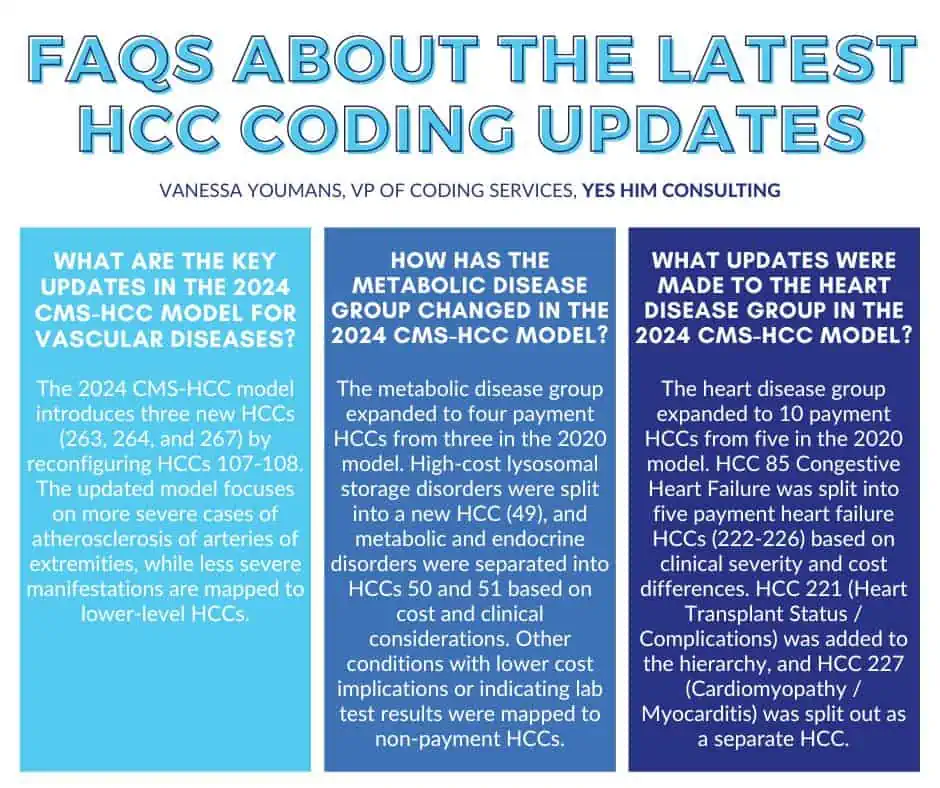
Delving into HCC
Within the CMS framework lies the Hierarchical Condition Categories (HCC) model, a nuanced system designed to assess patient risk and allocate resources accordingly. Think of HCC as a sophisticated algorithm that whirs silently in the background, calculating risk scores based on a patient’s medical history and diagnosed conditions. By stratifying patients’ health risks, the HCC model enables providers to receive appropriate reimbursement for the care they deliver, ensuring that providers are supported to manage their patients effectively.
The HCC model categorizes diagnoses into specific groups that reflect the severity and complexity of patients’ health conditions. Each category is assigned a corresponding risk adjustment factor, akin to a weighted score that reflects the likely cost of care for patients within that category. The significance of HCCs in medical billing cannot be overstated; they provide a framework for the reimbursement process that directly correlates with patient needs, taking into account not just the presence of a diagnosis but the intricacies of an individual’s health profile.
The Interplay between CMS and HCC
The relationship between CMS and HCC is symbiotic, forming an essential collaboration that enhances the infrastructure of healthcare funding. CMS utilizes the HCC model to determine payment rates for Medicare Advantage plans, making the choices of health plans more reflective of the populations they serve. This model aims to ensure that higher-risk patients, who typically require more extensive and costly care, are appropriately funded. Thus, it creates a more equitable distribution of resources, fostering a healthcare environment that caters to varied needs without the specter of inadequate funding.
This interplay also presents challenges. Providers must stay astute, adapting to changes in coding and billing practices that may arise as CMS evolves its guidelines. Accurate documentation and coding become paramount in this dynamic landscape. Every nuance in a patient’s medical history carries potential financial implications. Failing to capture the full spectrum of a patient’s conditions not only jeopardizes the financial viability of healthcare organizations but also compromises the quality of care patients receive.
Implications for Healthcare Providers
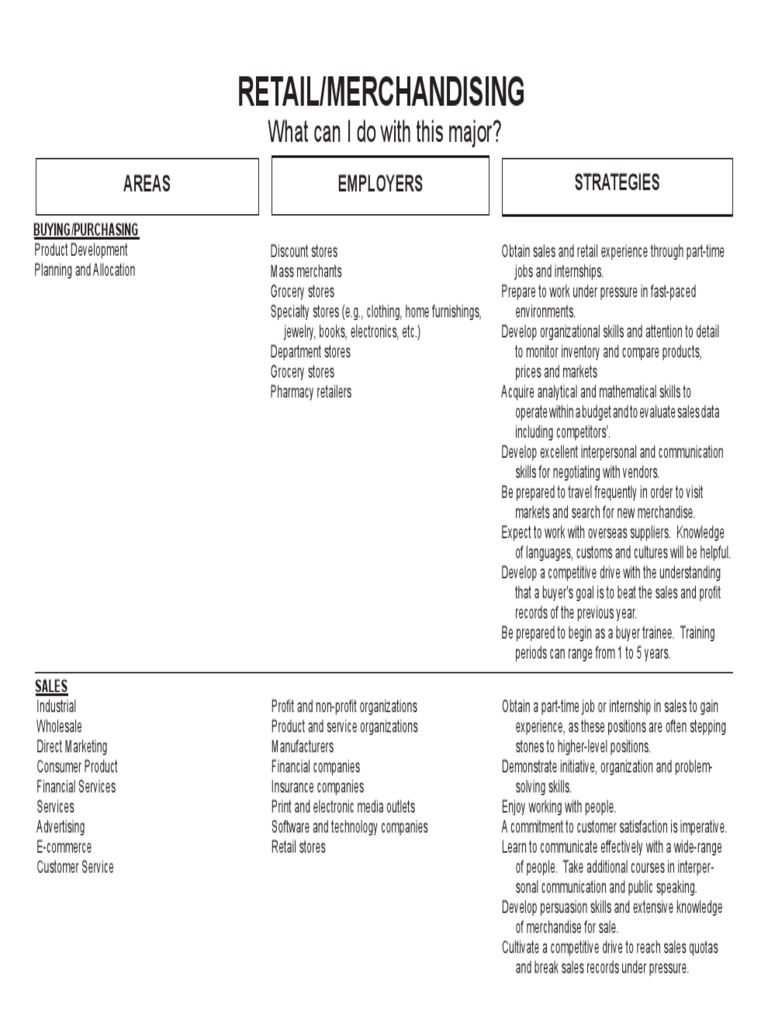
Healthcare providers are akin to architects constructing a robust healthcare system; their understanding and implementation of CMS and HCC principles can decide the stability of their practice and the quality of patient care. By comprehensively documenting patient histories and applying the HCC model adeptly, providers position themselves favorably within the reimbursement landscape. A nuanced approach can elevate a practice’s revenue by ensuring they are compensated for the complexities of the care they offer.
Moreover, involvement in programs such as value-based care—where reimbursement is tied to the quality of care rather than quantity—demands an even deeper comprehension of HCC principles. Providers are not merely treating ailments; they are curating a patient’s overall journey towards well-being, balancing costs and outcomes skillfully.
Importance for Patients
For patients, the ramifications of CMS and HCC extend beyond the realm of billing—they impact the very essence of their healthcare experience. Through the lens of HCC, patients with chronic or complex conditions can receive the attention and resources they need, ensuring their health trajectories are supported by appropriate funding. This alignment of financial resources with medical needs fosters an environment where patients can prioritize their health without the looming anxiety of financial burden from inadequate coverage.
Ultimately, the delicate dance of CMS and HCC shapes the landscape of healthcare accessibility and quality. The insights gleaned from understanding these systems illuminate the path toward a healthcare setting where providers are empowered to offer exceptional care, and patients can engage confidently in their health journeys.
In conclusion, CMS and HCC represent more than mere acronyms in medical billing; they encapsulate the very ethos of contemporary healthcare finance. Their nuanced interplay ensures that healthcare remains a responsive, adaptive system, capable of evolving alongside the ever-changing needs of patients and providers alike. Armed with this knowledge, stakeholders can navigate the complexities of medical billing, enhancing the experience and outcomes for all involved.