Dental hygiene is an essential component of overall health, yet it often garners less attention than it merits. As oral hygiene practices evolve and scientific understanding of oral health deepens, the importance of case studies in this field becomes increasingly evident. An exemplary case study serves not merely as a clinical report but as a narrative that encapsulates the complexities of patient care, the intricacies of oral health, and the socio-behavioral elements that underpin dental hygiene. In this exploration, we will delve into a specific case study that showcases the multidimensional aspects of dental hygiene and reflects on the underlying psychosocial factors that can elevate mundane oral care into a subject of fascination.
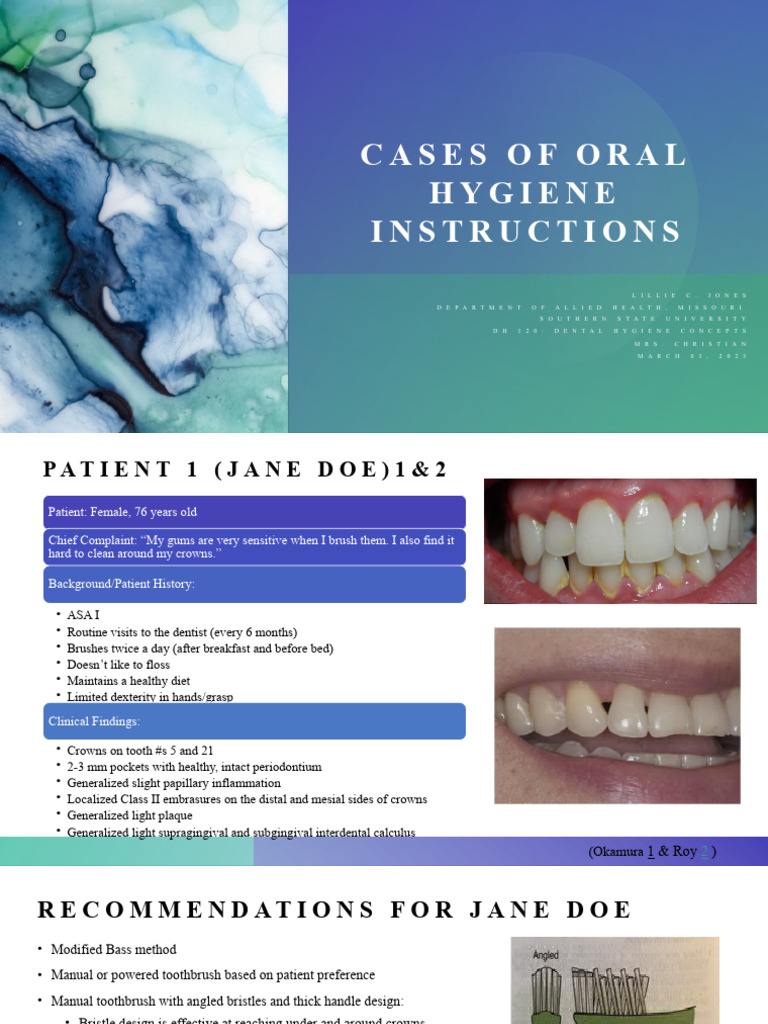
The case study of a 25-year-old female patient, whom we shall refer to as Sarah, provides a rich tapestry from which significant insights can be drawn. Upon her initial consultation, Sarah exhibited several common but critical issues: gingival inflammation, plaque accumulation, and a generally low level of oral hygiene quality. These manifestations raised immediate concerns regarding her long-term dental health, as well as potential systemic implications.
What catalyzed Sarah’s visit was her increasing awareness of discomfort in her gums, which had been exacerbated by her recent lifestyle changes—namely, a shift toward a more sedentary routine accompanied by a diet high in sugars and processed foods. This lifestyle pivot highlighted a common observation: the intricate relationship between dietary habits and oral health. Thus, the case study began by meticulously documenting her oral health history, analyzing dietary patterns, and identifying behavioral factors that potentially contributed to her condition.
To truly understand Sarah’s situation, one must explore the psychosocial dynamics at play. The propensity to neglect oral hygiene often stems from several deeper issues—stress levels related to work-life balance, lack of effective education on dental care, and socioeconomic factors that influence access to dental services. Sarah’s struggle was emblematic of a broader societal issue: how personal circumstances can color one’s approach to health. Her case aligns with a fascinating observation in public health; it is not merely about individual choices but a confluence of social determinants that can inspire or inhibit positive health behaviors.
The initial phase of Sarah’s treatment included a comprehensive dental assessment, coupled with clinical interventions such as scaling and root planing to manage her gingivitis. The immediate results were promising, as the reduction in plaque and inflammation laid the groundwork for a more sustained oral health regimen. Yet, it was during the follow-up consultations that the foundation of the case study truly began to flourish. Here, the significance of patient education became paramount—encouraging Sarah to embrace a more proactive approach toward oral hygiene.
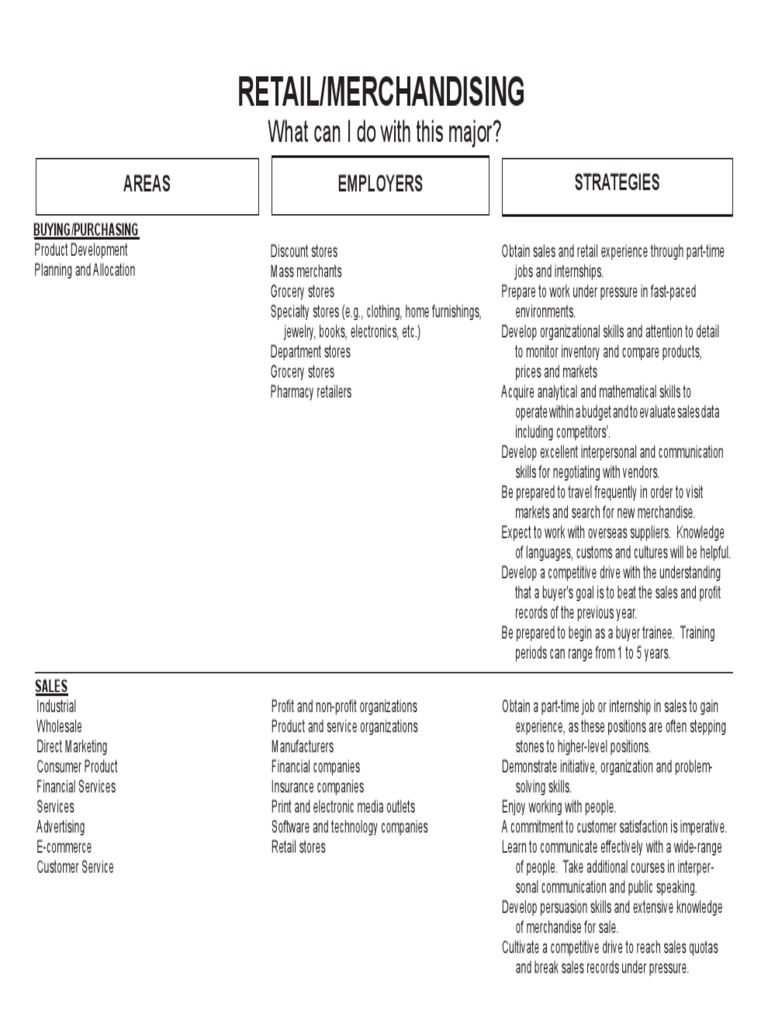
Implementing behavioral change, particularly in the realm of hygiene practices, necessitated more than mere recommendations. A tailored patient-centered strategy was adopted, which involved the formulation of personalized oral hygiene goals and the introduction of tools that would assist in maintaining her dental health. Sarah was introduced to the utility of electric toothbrushes and interdental tools, alongside flossing techniques designed to facilitate effective plaque removal.
However, an essential aspect of the case study was not merely the technical adjustments but also the psychological support provided to Sarah. Encouragement and moral support from the dental team played a crucial role in fostering her motivation. This raises a pertinent question about the therapeutic alliance in dental care: how do clinician-patient relationships inform the efficacy of treatment outcomes? Inspirational narratives often reveal that the path to sustainable health behavior is paved with consistent guidance, empathy, and understanding.
Throughout the course of treatment, periodic assessment of Sarah’s oral hygiene practices allowed for real-time tweaks to her regimen, ensuring that she remained engaged in her care plan. These interactions provided valuable data points to evaluate her understanding and adherence to the prescribed methods. For instance, discussions around her dietary choices reinforced the need to reduce sugar intake, illustrating the reciprocal relationship between nutrition and oral hygiene. By incorporating real-life strategies into her diet, such as opting for fibrous vegetables and rinsing with water post-snacking, Sarah began to see tangible improvements not only in her oral health but in her overall wellness.
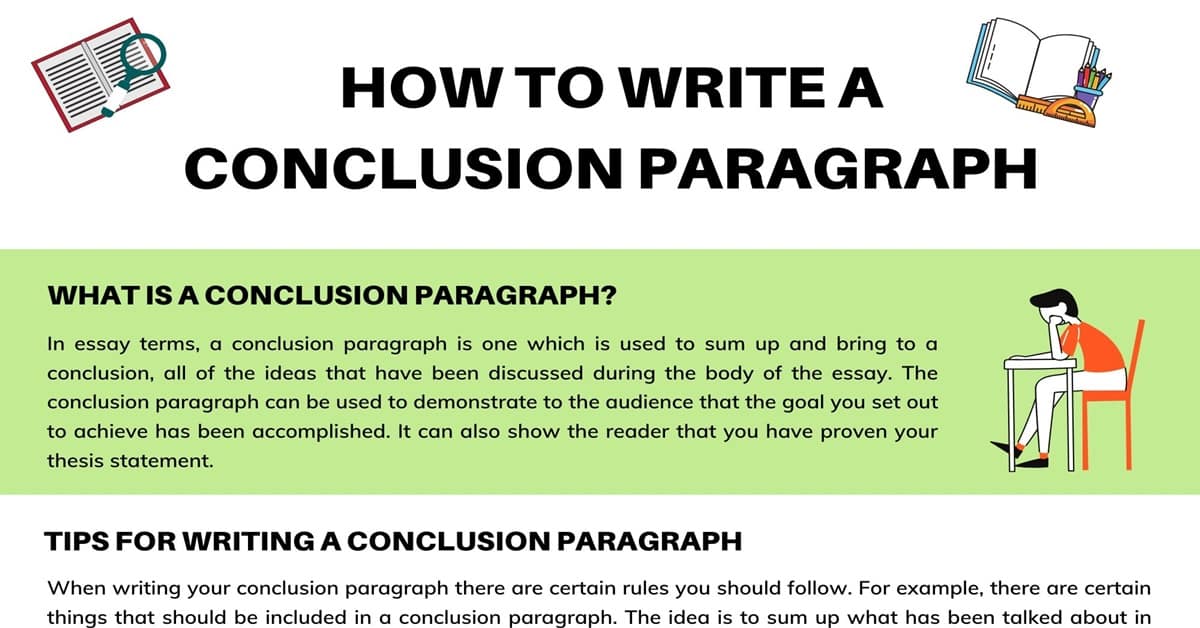
The culmination of Sarah’s case study exemplifies the transformative impact of holistic approaches in dental hygiene. Over the span of several months, monitoring revealed significant reductions in plaque accumulation and gingival inflammation. Yet more importantly, the case study illuminated the profound effect of education, empowerment, and emotional support on patient engagement. Sarah’s journey from discomfort to confidence stands as a testament to the power of personalized dental care.
In summation, this dental hygiene case study encapsulates more than clinical data—it illustrates the intertwined nature of health behaviors, personal circumstances, and professional care. It shows us that the story of oral hygiene goes beyond the surface of teeth and gums, delving into the intricate layers of human experience that dictate health choices. The examination of Sarah’s case compels professionals to consider how societal and psychological variables converge to shape oral health, and it underscores the necessity of comprehensive approaches tailored to the individual. The fascination derived from such observations only serves to accentuate the richness of dental hygiene as a field deserving of ongoing exploration and understanding.