Have you ever pondered the implications of a borderline ECG on an EKG? It’s a question that can ignite anxiety and curiosity alike. The heart is a magnificent organ, incessantly pumping life-giving blood throughout our body, and understanding its fluctuations can often feel daunting, especially when faced with the ambiguous nature of a borderline ECG reading. What does it really signify, and what challenges might it pose for your health? Let’s embark on a journey through the demystifying realm of electrocardiograms (EKGs) to uncover what a borderline ECG entails.
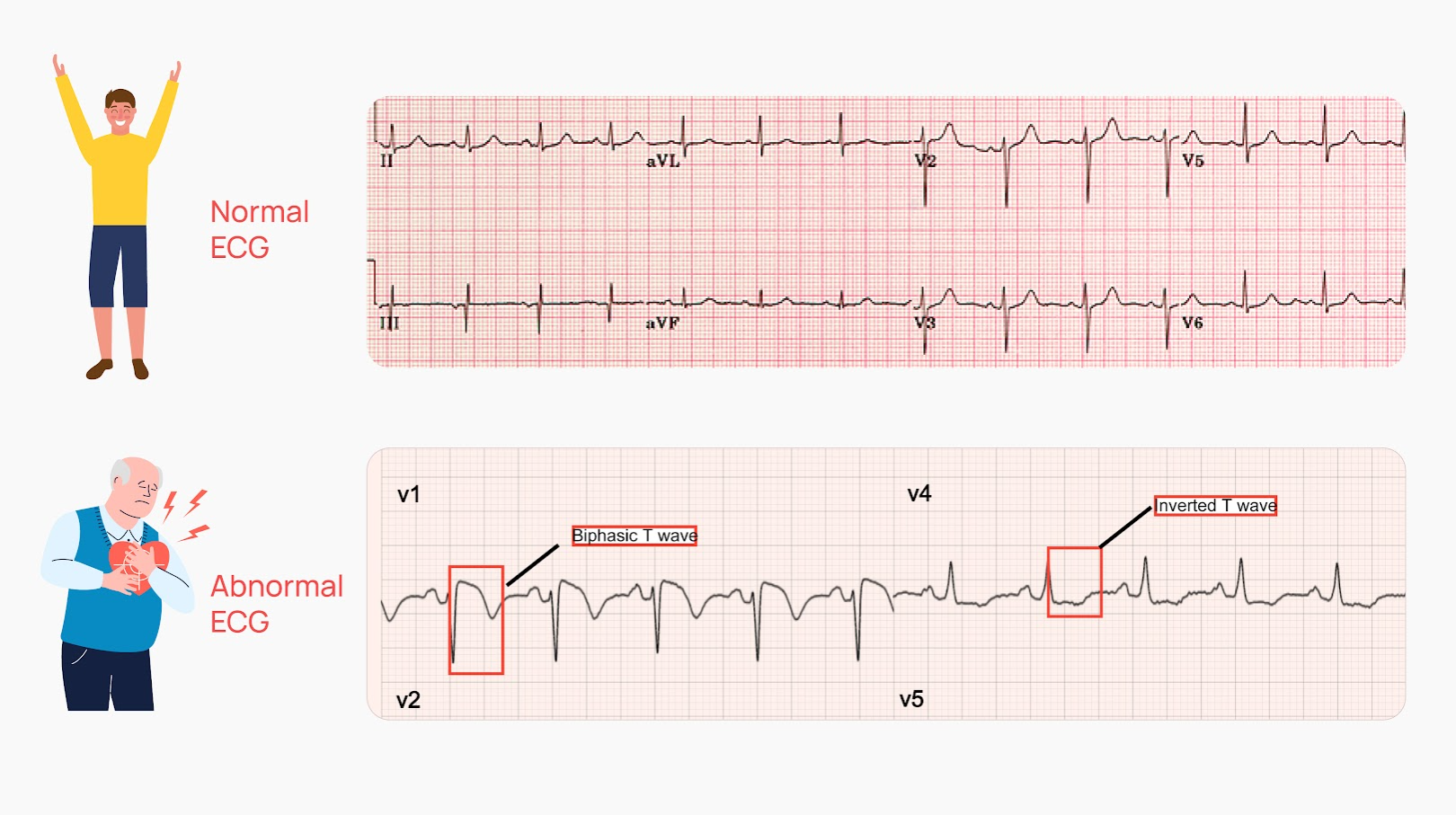
An electrocardiogram (EKG or ECG) is a diagnostic tool that captures the electrical activity of the heart, providing essential insights into its rhythm and functionality. The ECG is plotted on a graph, portraying waves and intervals that correspond to the heart’s beats and electrical impulses. But what happens when those readings land in the murky middle ground—considered borderline rather than firmly normal or unquestionably abnormal?
A borderline ECG may indicate that certain parameters fall outside the conventional range for a healthy heart, yet not severely enough to classify as a clear abnormality. This gray area can often lead to more questions than answers for both patients and healthcare providers. Could it be a sign of an underlying heart condition, or perhaps a fleeting quirk in the electrical pathways of the heart? Understanding the implications of this can be crucial for managing one’s heart health.
A multitude of factors can contribute to a borderline ECG. From age and sex to underlying medical conditions and medications, the spectrum is vast. Age, for instance, plays a significant role in ECG readings. As one ages, the heart’s electrical system goes through changes, potentially leading to variations that, while still “normal,” can straddle the borderline. Additionally, certain physiological states—like dehydration or extreme physical exertion—may induce transient changes that don’t signal any chronic heart issues.
Recognizing a borderline ECG also necessitates an understanding of the common components evaluated in the reading:
- Heart Rate: A normal resting heart rate should generally be between 60 to 100 beats per minute. Rates that deviate from this range may be considered borderline, potentially signaling bradycardia or tachycardia.
- Rhythm: The heart rhythm is characterized by regularity and pattern. A borderline evaluation might indicate an irregular heartbeat, such as occasional atrial fibrillation or premature contractions.
- Intervals: Key intervals, including PR, QRS, and QT intervals, are scrutinized for length. An elongation or shortening of these intervals can classify the ECG as borderline.
- ST Segment and T Waves: The morphology of these components can indicate whether the heart is under stress or experiencing ischemia, with borderline findings possibly hinting at potential future risks.
Of particular interest is how borderline ECGs can lead to further diagnostic endeavors. Upon receiving a borderline reading, clinicians may recommend additional tests to elucidate the heart’s condition. Echo-cardiograms and stress tests are frequently employed tools that provide supplemental data, offering a clearer picture of the heart’s anatomy and functionality under exertion. The potential challenge here is twofold: first, the anxiety that stems from uncertainty can feel overwhelming, and second, the need for further investigation might lead to additional costs and time investment.
Despite these challenges, navigating the landscape of a borderline ECG need not resemble traversing a minefield. It is rather a call for a more nuanced approach to heart health. Engaging with healthcare professionals to discuss your specific risk factors—such as family history of heart disease, lifestyle choices, and existing medical conditions— can empower you with knowledge. Are you sufficiently physically active? Is your diet conducive to cardiac health? Addressing these questions can foster a proactive attitude toward your heart health.
Moreover, understanding the implications of a borderline ECG opens avenues for lifestyle adjustments that can optimize heart health. Engaging in regular cardiovascular exercises, eating a heart-healthy diet rich in fruits, vegetables, and lean proteins, and managing stress levels through mindfulness or therapeutic practices can enhance your overall wellness. These lifestyle changes do not merely stabilize heart function; they create a foundation for long-term vitality.
Nevertheless, remaining vigilant about any symptoms that accompany borderline readings is crucial. Symptoms such as persistent palpitations, shortness of breath, or chest discomfort warrant immediate professional attention. These manifestations may not merely be side effects of anxiety; they could indicate underlying conditions that require timely intervention.
In conclusion, a borderline ECG presents intriguing questions and concerns—often a blend of challenge and opportunity for introspection regarding one’s overall health. While it may provoke apprehension, it also serves as a pivotal reminder of the critical role our heart plays in our health narrative. Comprehending the meaning behind a borderline ECG can empower individuals to take control of their heart health, thus turning uncertainty into actionable insights.
Are you prepared to heed the signals your heart presents? The journey to understanding your cardiovascular health begins with awareness.