Embarking on the journey of pregnancy is an exhilarating yet complex experience filled with a plethora of medical terminologies, inevitably leading to a few confusions along the way. One such abbreviation that often surfaces in discussions among expectant parents is “AF.” Understanding what AF stands for, particularly in the context of pregnancy, is essential for navigating through medical conversations, appointments, and literature.
AF generally refers to “Antepartum Fetal,” a term that encompasses various aspects of the fetal development stage prior to childbirth. It is pivotal to delve into the various connotations and applications of this abbreviation in order to grasp its significance in prenatal care.
**1. Defining Antepartum Fetal**
Antepartum refers to the period occurring before labor begins. In the context of fetal health, “Antepartum Fetal” encompasses numerous evaluations, assessments, and monitoring practices aimed at ensuring the well-being of the fetus during the pregnancy phase. The antepartum period typically spans from conception until the onset of labor, making it a critical time for medical oversight and intervention if necessary.
**2. Assessing Fetal Health: What to Expect**
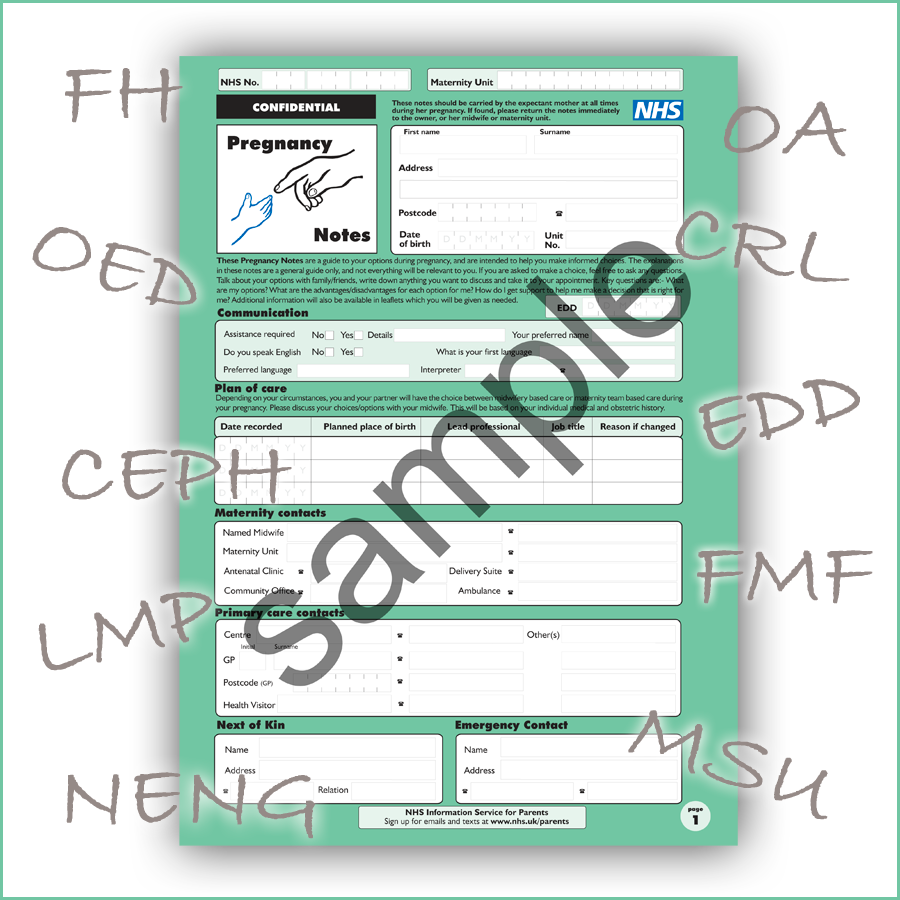
During the antepartum phase, expectant mothers undergo various medical evaluations to monitor fetal health. This includes routine ultrasounds, Doppler checks of fetal heart rate, and other non-invasive tests that provide insights into fetal development. These assessments serve to identify any potential anomalies early on, ensuring that both the mother and fetus receive appropriate care throughout the pregnancy.
Ultrasounds, a cornerstone of antepartum care, facilitate the visual examination of fetal growth, placental placement, and amniotic fluid levels. The frequency of these ultrasounds may increase in high-risk pregnancies, where vigilance becomes paramount due to factors such as maternal health conditions or advanced maternal age.
**3. Complications Discussed: Antepartum Assessment**
Antepartum assessments also extend to recognizing potential complications, such as gestational diabetes, preeclampsia, and intrauterine growth restriction (IUGR). By utilizing detailed maternal histories, screenings, and laboratory tests, healthcare providers can adeptly identify red flags that may require further investigation or intervention.
For instance, preeclampsia, characterized by high blood pressure and organ dysfunction, is often diagnosed through routine blood pressure monitoring combined with urinary protein checks during the antepartum period. Early detection is crucial because preeclampsia can escalate to serious health issues for both mother and child if left unaddressed.
**4. Support Systems: Building a Network**
Building a strong support system during pregnancy is equally important as the direct medical care received. It is advisable for mothers to engage with a network of healthcare professionals, ranging from obstetricians and midwives to specialized maternal-fetal medicine practitioners. Being informed about the latest research, medical practices, and community resources can profoundly affect decision-making and overall prenatal experiences.
Furthermore, joining prenatal classes or support groups can foster camaraderie among expectant mothers, allowing them to share experiences, insights, and advice on navigating the intricacies of antepartum care.
**5. Emerging Technologies in Fetal Monitoring**
As technology advances, so too does the field of prenatal care. Innovative tools such as fetal monitors and wearable devices have emerged, enhancing antepartum surveillance capabilities. These cutting-edge technologies facilitate real-time monitoring of fetal heart activity and uterine contractions, providing peace of mind for expectant parents and enabling prompt medical responses when necessary.
Moreover, telehealth options have gained traction, especially post-pandemic. Virtual consultations allow pregnant individuals to receive expert advice and assessments from the comfort of their homes, making antepartum care more accessible and less daunting.
**6. The Importance of Maternal Mental Health**
While physical health is paramount, mental well-being is an equally critical component of antepartum care. The emotional rollercoaster pregnant women often experience necessitates attention to their mental health. Conditions like prenatal anxiety and depression, while sometimes overlooked, warrant significant focus as they can impact both the mother’s and child’s health.
Healthcare providers should routinely screen for emotional wellness during prenatal visits, offering resources or referrals to mental health specialists when needed. Supportive counseling and engaging in self-care practices can help mitigate stress, promoting a healthier pregnancy environment.
**7. Preparing for Childbirth: The Transition from Antepartum to L&D**
As pregnancy progresses into the later stages, the antepartum period ultimately transitions into labor and delivery (L&D). Knowledge gained during the antecedent months equips expectant mothers for the imminent challenge of childbirth. It is imperative to formulate a birth plan, communicate preferences with healthcare providers, and remain informed about potential labor interventions.
Understanding the nuances of AF in the context of pregnancy can facilitate better preparation for the transformative experience of childbirth. Realizing the full scope of antepartum care allows expectant mothers to advocate for themselves and their baby effectively.
In summation, the abbreviation AF stands as a gateway into a profound exploration of antepartum fetal health. From assessments and monitoring practices to mental health considerations and technological advancements, the antepartum period is an intricate tapestry that lays the groundwork for successful childbirth outcomes. Understanding and embracing this terminology ultimately cultivates a more informed and empowered maternal experience.