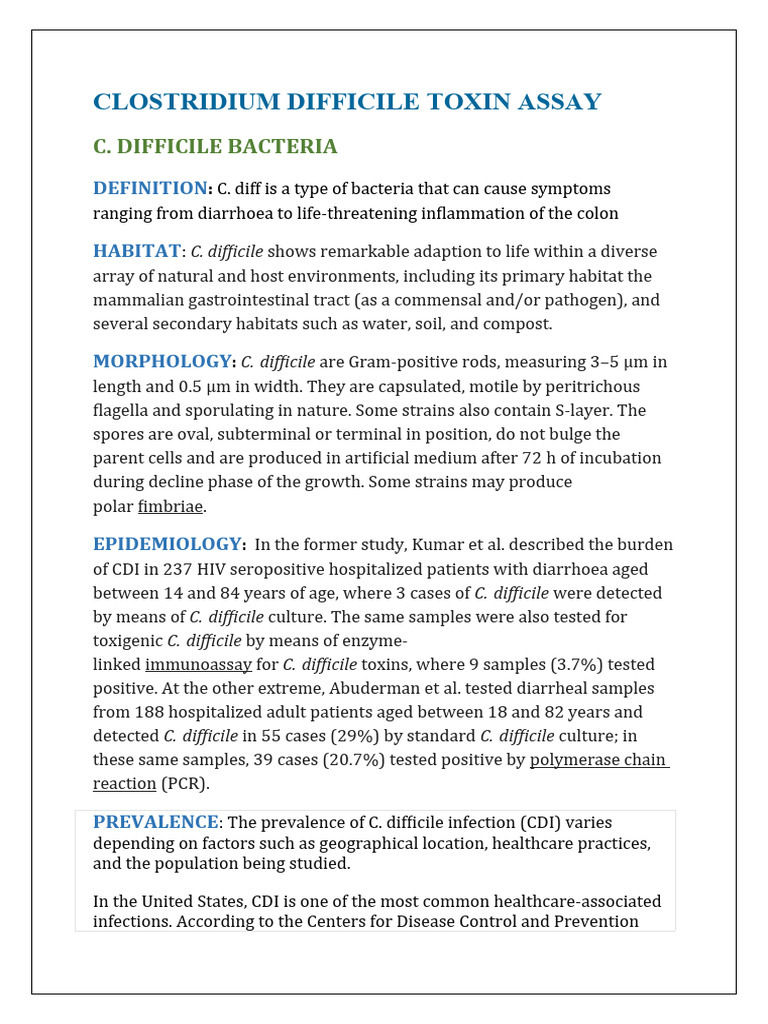
Clostridioides difficile, commonly referred to as C. diff, is a bacterium that causes significant gastrointestinal distress, often manifesting as diarrhea, abdominal pain, and fever. Among healthcare professionals and patients alike, the terminology surrounding C. diff can often lead to confusion, particularly when interpreting diagnostic results. A notable and frequently discussed result is the “C. diff antigen positive and toxin negative” finding. What does this mean, and why does it raise so many questions?
To delve into the implications of these diagnostic outcomes, it is essential to understand the microbiology of C. diff. This bacterium exists in various strains, some of which produce toxins—specifically toxins A and B—while others do not, or they may produce an antigen that indicates the presence of the bacteria without generating toxins. Hence, a positive antigen test signifies that the organism is present, but a negative toxin test raises an eyebrow; it suggests that although C. diff is detected, its harmful toxigenic activity may not be occurring.
The first port of call in unraveling this complex phenomenon is to comprehend the nuances of the diagnostic tests themselves. The antigen test typically detects the presence of a specific protein associated with the C. diff organism. When a test returns positive, it implies that C. diff is present in the stool. Conversely, the toxin test directly checks for the pathogenic substances the bacteria produce. A negative result here indicates that while the bacterium is not expelling its virulent toxins at the moment of testing, it may still be present in a dormant or non-toxigenic form.
This raises a compelling question: What does it mean for a patient to be antigen positive yet toxin negative? Unquestionably, it complicates the clinical picture. Clinicians are thus faced with the critical task of determining the next steps. In many cases, this result is termed as “asymptomatic carriage”. This phenomenon can often be observed in patients who may have previously undergone antibiotic therapy or those with other underlying conditions that influence the gut microbiome.
Understanding the implications of a C. diff antigen positive and toxin negative result compels one to consider the broader landscape of gut health. The gastrointestinal tract is a complex ecosystem, home to trillions of microorganisms, collectively known as the microbiome. An imbalance in this microbiome, often exacerbated by antibiotic usage or hospitalization, can lead to opportunistic infections like C. diff. In this context, a positive antigen result is far more than an isolated lab finding; it can be an indicator of broader microbiome disruption.
As we ponder this diagnosis further, it becomes paramount to consider the subsequent steps in patient management—clinical correlation is key. Just because a patient has a positive antigen and negative toxin finding doesn’t automatically warrant aggressive intervention. In cases where patients present with no clinical symptoms, clinicians may choose to monitor the individual rather than initiate treatment. However, when symptoms arise, the focus turns to more definitive testing, vigilant assessment, and potential therapeutic interventions.
Moreover, clinicians are now armed with a plethora of guidelines that assist in navigating these ambiguous waters. The presence of symptoms, in conjunction with laboratory findings, aids in determining whether a patient is a candidate for operative treatment versus conservative management. For example, if the patient showcases signs of severe colitis or dehydration, immediate treatment becomes necessary regardless of the toxin test outcome.
In the intricate narrative of C. diff diagnostics, one must also highlight the importance of patient education. Understanding the distinction between antigen positivity and toxin negativity offers patients a clearer insight into their health status. This enables them to engage actively in conversations about their treatment options while emphasizing the importance of maintaining a balanced microbiome post-diagnosis. Probiotics, dietary modifications, and cautious antibiotic usage may play pivotal roles in ensuring a healthier gut environment.
While C. diff antigen positive and toxin negative may initially provoke concern, it can also be an opportunity for exploration into the evolving frontier of infectious disease treatment. The emergence of novel therapies and the potential for using fecal microbiota transplantation—where healthy gut flora is introduced to restore balance—could reshape the handling of such cases in the future. Researchers continue to explore how to best mitigate the risk of C. diff infections even in the context of existing pathogenic bacteria.
Ultimately, the discussion surrounding C. diff antigen positivity and toxin negativity is not simply a clinical curiosity. It embodies a more profound contemplation of the intricate interplay between pathogens and our underlying health. Understanding these diagnostic nuances invites both healthcare professionals and patients alike to consider the multifaceted nature of health and disease. It encourages an active dialogue about maintaining microbial balance, the significance of holistic care, and the evolution of treatment methodologies in our modern healthcare landscape.
In conclusion, while C. diff antigen positive and toxin negative results may raise immediate questions regarding management, it serves as a catalyst for further inquiry into the depths of gastrointestinal health. As our understanding of the microbiome expands, so too does our capacity to effectively address these complexities, ultimately leading to better patient outcomes and enhanced quality of care.