In the intricate tapestry of medical discourse, the phrase “clinically correlate” often emerges as a linchpin, drawing attention to the symbiotic relationship between clinical findings and imaging studies. This term can feel cryptic to those unacquainted with the nuances of medical jargon, yet understanding its implications is pivotal for both healthcare providers and patients navigating the labyrinthine world of medical diagnosis and treatment. This article endeavors to illuminate what “clinically correlate” entails and why it matters, thereby demystifying a potentially confounding aspect of medical reports.
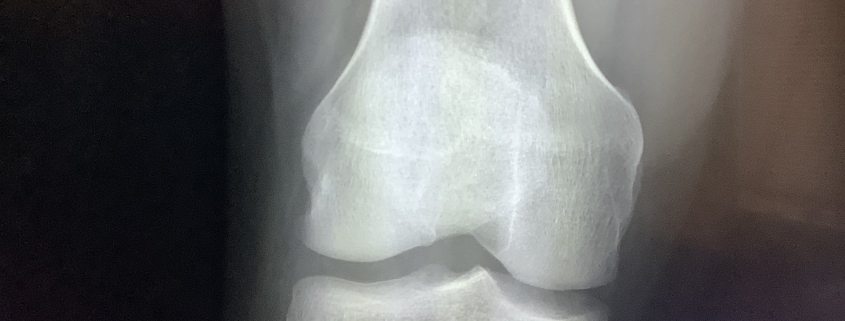
At its core, “clinically correlate” signifies that the findings observed in imaging tests, such as X-rays, MRIs, or CT scans, must be interpreted in the context of the patient’s clinical symptoms or history. It encourages a holistic approach to patient care, where disparate fragments of medical data coalesce into a coherent understanding. The very essence of correlation in this instance is akin to the intricate dance of shadows and light—where one cannot exist without the other for a complete picture of health to emerge.
The Importance of Context in Radiology
In radiological reporting, physicians often encounter a variety of findings that may appear alarming or significant when viewed in isolation. However, unless these findings resonate with the patient’s clinical landscape, their relevance can be overstated or misunderstood. The directive to “clinically correlate” serves as a powerful reminder: imaging results are not standalone artifacts but rather components of a larger clinical narrative.
For instance, consider a scenario where an MRI reveals a benign lesion in the brain. If the patient exhibits no neurological symptoms—such as headaches, seizures, or cognitive disturbances—the finding may be deemed clinically insignificant. Conversely, if the same lesion is found in a patient with ongoing neurological deficits, the interpretation shifts dramatically, heralding a potential need for further investigation or intervention. This underscores the necessity of contextual acuity; the delineation between alarming and benign can often pivot on clinical correlation.
The Interplay Between Symptoms and Imaging Findings
Simplistically, the dynamic between symptoms and imaging findings embodies a complex interplay. Symptoms serve as the initial signals that alert physicians to potential maladies, guiding them to choose the appropriate imaging studies. The results of these tests, in turn, can confirm, refute, or complicate the preliminary diagnosis initiated by the symptoms.
To illustrate this interplay further, imagine a patient presenting with chest pain. An electrocardiogram (ECG) initially suggests a myocardial infarction; however, subsequent cardiac imaging adds a layer of complexity by indicating a pericardial effusion, a situation better understood when viewed through the lens of clinical correlation. Symptoms alone may mislead; imaging results devoid of symptom context could steer the clinical approach amiss. Thus, clinical correlation is tantamount to an essential checkpoint along the diagnostic pathway.
Interdisciplinary Collaboration and Clinical Correlation
Efficient clinical correlation extends beyond individual practitioners into the realm of interdisciplinary cooperation. Radiologists and clinicians must engage in ongoing dialogues that clarify diagnostic goals and treatment options. This collaboration often leads to a richer interpretation of imaging findings, ultimately enhancing patient outcomes.
Take, for example, the oncology domain. Imaging tests—such as PET scans—may reveal metastatic growth in a patient’s liver. However, the implications of this finding can vary drastically based on the patient’s cancer history, treatment responses, and symptomology. Engaging both oncologists and radiologists ensures that the imaging is interpreted not merely as an isolated concern but as a significant factor in a broader treatment strategy. In such scenarios, clinical correlation acts as a synergistic glue, fostering a deeper understanding of the patient’s comprehensive medical narrative.
The Impact of Advanced Imaging Technologies
With advancements in imaging modalities, the potential for finding incidentalomas—unexpected findings—has surged. These incidental findings, while frequently benign, can unleash a torrent of challenges regarding clinical correlation. The high resolution and detail provided by modern imaging techniques can sometimes expose anomalies that prompt further investigation.
This raises critical questions regarding the appropriate response to such findings. Do they merit immediate intervention? Or, can they be safely monitored within the context of the patient’s overall health? Here, once again, the principle of clinical correlation becomes indispensable, guiding healthcare providers toward prudent and calibrated decision-making.
Patient Experience and Clinical Correlation
From the patient’s perspective, the phrase “clinically correlate” can provoke feelings of uncertainty, as it often implies that more information and interaction are necessary for a definitive diagnosis. Patients, after all, seek clarity and reassurance in moments of distress. Engaging in clear communication regarding the significance of clinical correlation is essential. By demystifying medical language and exploring the rationale behind the need for correlation, healthcare providers can foster trust and alleviate anxiety.
The journey towards understanding one’s health is inherently complex and layered. Inherent in this complexity is the need for ongoing discussions about various findings, an acknowledgment that no result exists in a vacuum.
Conclusion: The Path Forward
In a healthcare environment increasingly defined by technological sophistication, the essence of “clinically correlate” remains a cornerstone. It embodies the interplay between symptoms and diagnostic tools—an indispensable paradigm for accurate, effective patient care. Moreover, it emphasizes that every imaging result, every symptom must be woven into the rich fabric of the patient’s unique health narrative. Embracing this holistic view not only enhances diagnostic precision but also underscores the profound impact of context in understanding health and disease.