In the realm of healthcare, particularly within the confines of a hospital, terminology can oftentimes become a labyrinthine construct teeming with specific definitions and implications. Among the plethora of acronyms and medical codes exists an imperative designation: “Full Code.” This term delineates the extent to which medical personnel will employ life-saving measures in the event of a patient experiencing a critical decline in health. As we delve deeper into this crucial topic, we will unravel the intricacies of life-sustaining interventions, alternative codes, and the underlying ethical considerations involved.
Understanding Full Code: Definition and Overview
“Full Code” is a directive indicating that a patient desires or requires all resuscitative measures should their heart stop beating or they cease to breathe. This includes chest compressions, intubation, defibrillation, and the administration of medications designed to rejuvenate cardiac function. It is a commitment to pursue all available life-saving endeavors with the utmost intensity, reflecting a profound belief in the sanctity of life, and a refusal to concede to mortality without fight.
The Spectrum of Medical Codes: A Hierarchical Perspective
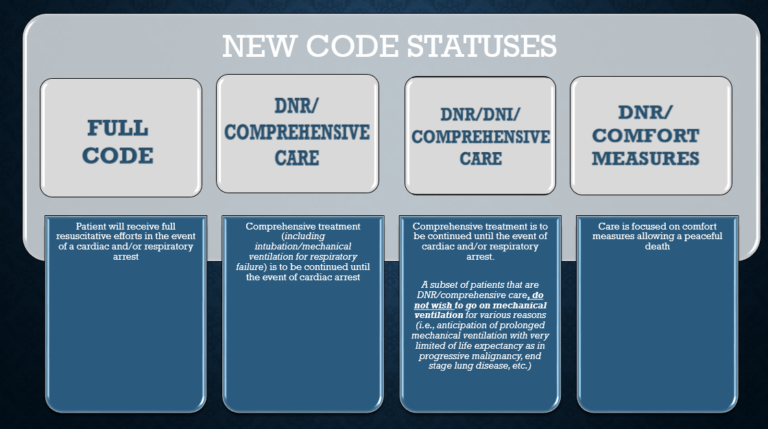
Within the sphere of resuscitation orders, it is pivotal to understand that “Full Code” is but one end of a varied spectrum. Medical directives, often categorized into different codes, represent a patient’s preferences regarding the extent of medical intervention. Common terminologies include:
- Full Code: As previously mentioned, this denotes a patient’s explicit consent to utilize every possible intervention.
- Do Not Resuscitate (DNR): A designation where the patient desires to forgo resuscitative efforts during cardiac arrest. This can stem from various reasons, including quality of life considerations or terminal illness.
- Allow Natural Death (AND): A more empathetic term often used in lieu of DNR. It emphasizes the acceptance of death as a natural conclusion of life and advocates for comfort measures rather than aggressive interventions.
- Selective Code: A less common order that approval for some but not all resuscitation efforts—this could mean that compression may be permissible but intubation is not.
These medical orders encapsulate the ethos of patient-centered care. They strive to honor individual values and preferences while ensuring informed decision-making steers the course of treatment.
The Importance of Communication and Documentation
Communication regarding resuscitation orders is paramount. Decisions about “Full Code” status should be articulated clearly among healthcare providers, patients, and their families to limit potential misunderstandings. It is vital that patients engage in candid discussions with their healthcare team to comprehend the implications of their choices. Optimally conducted, these conversations can foster informed decision-making, allowing patients to articulate their wishes without ambiguity.
Ethical Considerations Surrounding Full Code Orders
The ethical dimensions of resuscitation orders bear significant weight in clinical practice. The decision to be a “Full Code” may be influenced by numerous factors, including cultural beliefs, religious considerations, and personal values. Ethics committees within hospitals can provide essential support in navigating these complex conversations. They can aid patients and families in identifying their values, weighing treatment burdens against potential benefits, and comprehending the futility or efficacy of resuscitative efforts under various circumstances.
Case Studies: When Full Code May Be Challenged
Real-world scenarios often illustrate the challenges that arise surrounding “Full Code” orders. For instance, consider a patient who is in the advanced stages of a debilitating disease, where resuscitation may offer little more than temporary prolongation of suffering. In such cases, healthcare providers might advocate for a reconsideration of a “Full Code” status, encouraging a shift to more palliative measures that prioritize comfort above aggressive interventions.
Another illustrative case involves patients suffering from acute, reversible conditions versus chronic, irreversible ailments. Emergency departments often face dilemmas when treating patients with conflicting or unclear wishes regarding resuscitation, highlighting the necessity of precise documentation and communication among multidisciplinary teams.
The Role of Advance Directives and Living Wills
Advance directives and living wills serve as essential tools in articulating one’s medical treatment preferences, including resuscitative measures. A living will delineates a person’s wishes with respect to their medical care, particularly at times when they may become incapacitated. These documents enable patients to assert their autonomy even in futures where they may be unable to communicate their preferences.
Furthermore, legal ramifications can be significant. Healthcare providers are often obligated to honor the patient’s expressed wishes as documented in advance directives. Therefore, it is prudent for individuals to ensure that these documents are regularly reviewed and updated to reflect their current values and wishes.
The Final Insights: Embracing Patient Autonomy
In conclusion, “Full Code” represents a critical element within the intricate dance of hospital medicine, where the preservation of life often clashes with quality considerations and ethical dilemmas. Educating patients and families about their choices fosters advocacy and empowerment, ensuring that their values are represented in their treatment plans. The importance of maintaining clear, comprehensive dialogues surrounding resuscitation orders cannot be overstated. Ultimately, whether one chooses “Full Code” or another designation, the priority should always remain on aligning medical interventions with individual values, preferences, and the inherent dignity of life itself.